What is antimicrobial resistance?
Antimicrobial resistance (AMR) occurs when germs (bacteria, fungi, or viruses) no longer respond to medicines. Resistant germs can spread between humans, animals, and the environment.
AMR happens naturally over time, usually through genetic changes that occur within the germ. Resistance can increase by overuse or misuse of antimicrobials. Antimicrobials are treatments like antibiotics, antifungals, and antivirals.
AMR is one of the World Health Organization's (WHO) top 10 global public health threats facing humanity. It kills more than one million people around the world each year. The WHO predicts 10 million people will die annually from AMR unless appropriate action is taken now – that's higher than the number of people who die from cancer every year.
Drug-resistant infections can cause disease that is difficult or impossible to treat. They can even be fatal. In animals, this leads to poor animal welfare, pain, and production losses. Treatment costs can be greatly increased for both humans and animals.
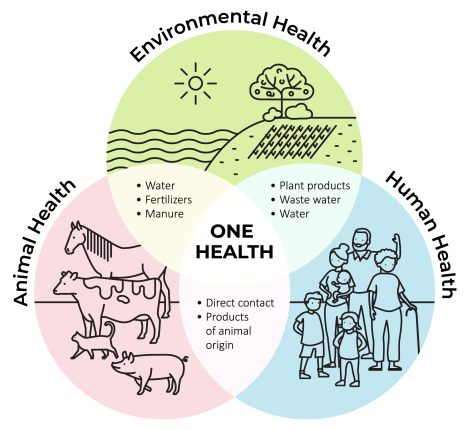
Antimicrobial resistance is a One Health issue
AMR can spread between animals, people, plants, and the environment. AMR is recognised to be a 'One Health' issue. One Health is a concept that recognises the interconnection between people, animals, plants, and their shared environment. One Health issues require collaboration at a local, regional, national, and global level.
Prevention and control of AMR in New Zealand
New Zealand Food Safety has an antimicrobial resistance work programme and in late 2022, it established an AMR team. The team is working towards the goals of the New Zealand Antimicrobial Resistance Action Plan. The AMR work programme includes:
- AMR surveillance
- monitoring
- auditing
- regulatory reassessment of antimicrobials
- education to promote stewardship of antimicrobials used in plants and animals.
You can email the AMR team at AMRteam@mpi.govt.nz







